Influenza season peaks early
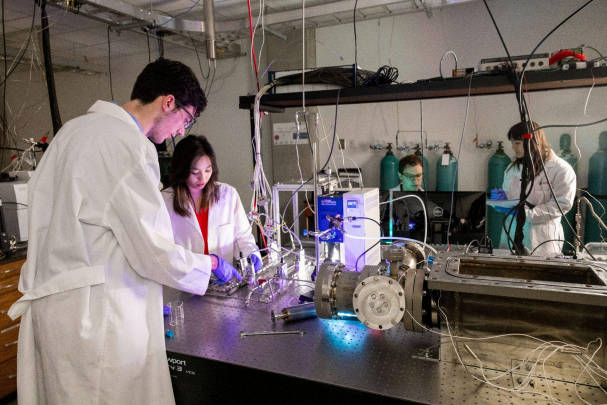
Emergency departments manage many patients with serious complications of the flu, sometimes having to send especially ill patients to the ICU.
January 24, 2020
More than 8,000 people in the U.S. have died of influenza this flu season, according to the CDC.
According to experts at the Centers for Disease Control and Prevention, there’s a 90-percent chance the flu season has peaked this winter. Last winter, the flu season claimed an estimated total of 80,000 lives. This was a record death toll in at least four decades.
Dr. Varun Phadke, who works with infectious diseases at Emory University Hospital, agrees with the CDC’s estimation.
“We certainly are seeing more influenza activity earlier in the year than previous years,” Phadke said. “We are also seeing more widespread, and by widespread, I mean more communities affected simultaneously with flu than usual at this time of year.”
He has also noticed another trend in the virus this year.
“Influenza B, which usually peaks substantially later in the year, like March or April, is actually peaking much earlier,” Phadke said. “This year, it seems to be the more predominant strain of flu, and it peaked in December and January.”
People may not know the common difference between the strains, but each come with their own attributes that affect the population differently.
“Influenza A is usually the one prone to cause pandemics and epidemics, and the reason for that is because Influenza A is the virus that could exist in more than one species of animal,” Phadke said. “Because of its ability to circulate in different species, novel strains of the virus can emerge that have pieces of viruses from other animals, and affect a population that had never seen those other viruses before. Influenza B is largely a human virus only, and so it doesn’t have that ability to pick up new pieces of genetic information.”
The prevalence of the B strain doesn’t pose as large of a threat because the normal symptoms attributed to the A strain are subdued in the B strain. However, Dr. Phadke finds it odd that despite the B strain being milder, this is still progressing as a peak year for the virus.
A big player in sending about 2.5 million people to the hospital this year alone due to the flu is the re-emergence of the subtype of the A strain: Type A H3N2. Once a new pandemic of the flu emerges, that subtype remains prevalent for a number of years after, before being replaced by a new pandemic and subsequent subtype.
“After the last pandemic, H3N2 predominated for a long time, until they were replaced by H1N,” Phadke said. “Usually, what we have observed in the last 10 or 11 years since the 2009 pandemic is that H1N1 viruses alternate every couple of years with an H3N2 season.”
Not only are the statistics showing the rapid progression of the flu, but individual Grady students are experiencing the effects of this virus.
Junior Zoey Phillips watched as members of her family fought symptoms of the flu.
“Over winter break, I went to visit my grandparents and cousins in Virginia,” Phillips said. “My cousin, Nicholas, wasn’t feeling well when they first arrived.”
But, what started out as a moment of weakness due to a prior injury progressed into something more serious.
“By that night, he had a fever of 101 degrees … and didn’t even have enough strength to pour himself a glass of water, let alone sit up straight,” Phillips said.
The Phillips family was forced to keep Nicholas quarantined, as they feared that he would infect her grandparents. In the end, it took him nearly a week to fully recover. Unfortunately, this wasn’t the end of the flu’s war path through the Phillips family.
“Five days later, my dad got sick, and suffered from a super bad cough and pain spread into his chest,” Phillips said. “He is still trying to get over his cough right now.”
She noticed a correlation upon realizing that her father had never received the vaccine and other members of the family had.
“My mom and I got the flu vaccination and only dealt with some small symptoms of a cold, like congestion and sore throats,” Phillips said.
The vaccination for the flu is also something that is a topic of concern. Experts are still debating on what strains to put into next season’s vaccine.
“Influenza is seasonal, and it circulates in the winter time in the northern hemisphere and our summer time in the southern hemisphere, and every year the strain of influenza circulating in the community changes a little bit from the year before,” Phadke said. “In order to make a perfect influenza vaccine, the manufacturers need to predict what strain is going to be circulating in the coming season.”
Just this year, school nurse Wanda Taylor helped Grady partner with Health Heroes to bring vaccines to students wanting to avoid contracting influenza.
“They contacted me and asked me if I’d like to have a flu clinic, and so I talked with Dr. Bockman (Principal Dr. Betsy Bockman), and she thought it sounded like a good idea,” Taylor said. “They came in with a nurse and a representative … and stayed from 10:00 in the morning until 2:00 [p.m.], and students … and staff came in to receive their flu shot.”
About 27 individuals were administered the shot, and although this is only its first year running, Taylor hopes the shots can be provided in the future.
“I thought it went well, but people thought it was going to be a continuous thing or that they were going to be able to come every day,” Taylor said. “But it was a one time deal.”
Phadke has a key set of responses when dealing with patients on the fence about receiving the shot.
“To that, I say all of the symptoms are a manifestation of your immune response to the vaccine,” Phadke said. “One could make the argument that the more potent that immune response, the more crummy you’re going to feel, but that also probably means that you’re mounting a powerful response to the vaccine that will protect you when you actually get exposed to the flu.”
Health experts like Dr. Phadke would argue that during this “peaking” flu season, it is best for everyone to be on high alert about symptoms their bodies present. The prevalence of a more lethal strain this year is setting the stage for more flu related hospitalizations. The most recommended way to prevent the flu would be vaccination.
“I spend time working in the clinic and in the hospital, and every year during influenza season, I see young, healthy people in the hospital, in the ICU on a ventilator because of influenza … which could’ve been entirely prevented if they had gotten the vaccine,” Phadke said.